How to Select the Best Value-Based Care Models for Post-Acute Physician Practices
Recently, Netsmart hosted How to Select the Best Value-Based Care Models for Post-Acute Physician Practices, a webinar presentation by Tom Haithcoat, president of Ceptor Consulting.
Tom’s association with post-acute care (PAC) stretches all the way back to his pre-teen years when he was a volunteer at a large county nursing home in his native Indiana. He has served in business development and management positions for national and regional skilled nursing organizations. In 2008, he transitioned to managing post-acute physician practices, and assisted in forming the Practice Group Network (PGN) in AMDA. In addition to his position with Ceptor Consulting, Tom is also president of Physicians Services Careline Health Group and serves on the AMDA board of directors.
Tom’s presentation covers why PAC physician practices need to focus on value-based care (VBC) solutions in post-acute health and how to choose the appropriate ones. Here’s a summary of some of the key points of this hour-long webinar.
CMS is Very Clear About its Commitment to Value-Based Care
It would be an understatement to say there’s confusion in US healthcare. But one thing is certain: fee-for-service (FFS) payment is on the wane and the Centers for Medicare and Medicaid (CMS) will remain dedicated to value-based care (VBC) and alternative payment models. CMS made that very clear in 2021 by establishing a goal to transition all Medicare beneficiaries to some type of value-based care solution for payments by 2030.

CMS has been preparing for this shift for quite a long time, starting with the Physician Quality Reporting System (PQRS) in 2007. PQRS provided an incentive payment for eligible physicians who satisfactorily report data on quality measures for covered services furnished to Medicare Part B FFS beneficiaries.
The marketplace is responding to this focus, as evidenced by these 2023 statistics regarding Medicare beneficiaries:
- 700,000 healthcare providers and facilities are participating in one of three VBC models
- 13.2 million beneficiaries aligned with some type of VBC model
- 28.4 million beneficiaries are in Medicare Advantage plans
- Only 17 million traditional Medicare beneficiaries remain
For PAC physician practices that haven’t yet ventured beyond FFS payments, it’s time to figure out which Value-Based Care model will work best for them and prepare for the transition. CMS takes a carrot-and-stick approach to encouraging adoption of new regulations. For example, early adopters of PQRS and electronic health records (EHRs)
received bonuses for figuring out how to implement the necessary technology and changes.
But it’s a one-way path from the carrot to the stick. The longer that practices wait, the more likely that quality performance models will no longer offer incentives, and eventually CMS will impose penalties. The writing on the wall is clear: change to a value-based care model while it’s still about benefits, and avoid the penalties that are sure to come.
Where Should PAC Physician Practices Start?
Take a look at your practice’s Total Per Capita Costs (TPCC), which measures the overall cost of care provided to beneficiaries as identified by your unique Taxpayer Identification. Number/National Provider Identifier (TIN-NPI). Your TPCC for attributed patients should be around 1:1 with the CMS average -- in other words, your costs are in line with what other practitioners are spending on their Medicare patients. If your TPCC is higher, dig in and find out what areas you need to improve.
Using this information, you can better assess where your current overall performance and what the results might be when you move to programs where your practice is exposed to risk in the form of real dollars. If you’re unable to easily access this information for your reference, it may be time to invest in better healthcare data analytics solutions.
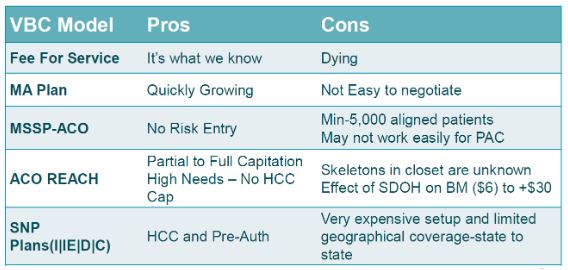
A Quick Review of Value-Based Care Models
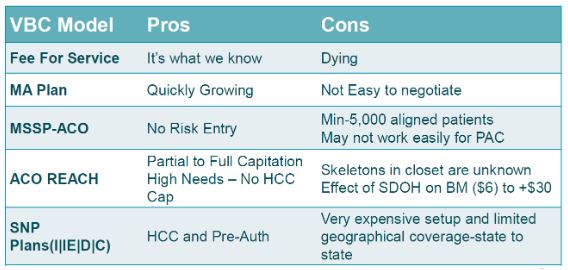
Medicare Advantage
Medicare Advantage plans are the fastest growing segment of patients transitioning to Value-Based Care solutions.. For PAC practices, however, the volume of patients simply isn’t high enough to have much leverage with insurance companies, so it’s difficult to negotiate much more than a glorified FFS arrangement.
Medicare Shared Savings Programs (MSSP)
Medicare Shared Savings Programs (MSSP) are permanent ACO programs in traditional Medicare that provide financial incentives for meeting or exceeding savings targets and quality goals. MSSPs offer multiple tracks that allow choosing between sharing in both savings and losses, or just savings. Practices can start with a no-risk period to get a feel for the flow of data and how to set up systems to adjust accordingly, so there is limited risk for entry. However, there are significant operational expenses and participants must have a minimum of 5,000 aligned patients.
ACO REACH
ACO REACH
is a newer shared-savings model designed to reach underserved communities. It offers a high needs component with complete capitation, a payment arrangement for healthcare services in which a physician or group of physicians receives a risk-adjusted amount of money for each person attributed to them, per period of time, regardless of the volume of services that person seeks. High needs is defined by risk adjustment factor (RAF) score or hierarchical condition category (HCC) coding, a risk-adjustment model originally designed to estimate future health care costs for patients. The efficacy and drawback for this model are not well known because it is new, so it is difficult to give exact details on the long-term effects of this value-based care model.
Special Needs Plans (SNPs)
Special Needs Plans (SNPs)
is a type of Medicare Advantage plan that combines all the benefits of original Medicare (Parts A and B) with prescription drug coverage (Part D) but is only available to those beneficiaries who have an additional qualifying condition. Those conditions include living in a long-term care institution (I-SNP), specific severe or disabling chronic conditions (C-SNP) and dual eligibility for Medicare and Medicaid (D-SNP).
SNPs can be advantageous for PAC practices because they use Hierarchical Condition Categories (HCCs) to project the expected risk and future annual care costs. However, there are geographical issues for practices that span state lines. SNPs are also expensive to set up and can incur considerable administration costs
Of these models, MSSP-ACOs may hold the most promise for PAC physician practices, but they must be mindful of how patients are attributed and other nuances that could cause issues.
Keeping an Eye on the Details
PAC providers also need to be cognizant of the special circumstances presented by their practices. For example, annual wellness visits are often cited as critical to participating in value-based care models. It’s certainly a good place to capture additional risk factors, get a holistic view of a patient and gather key insights and information at least once per year. That is certainly true for hospital associations and community-based models whose focus is patient engagement because they may only see a relatively stable patient two or three times a year.
However, PAC providers see patients as many as 12 to 15 times per year. Engagement isn’t as much of a concern as what happens in those visits, such as discussing goals of care and the trajectory of the patient’s condition. Tom offered a real-world example of how those discussions can impact care and costs.
His organization manually gathered patients’ code status and mapped it to overall costs and found a 50% reduction in overall costs for patients with no code vs. full code. He attributed that difference to understanding that full code vs. no code means more than whether to do chest compressions if a patient’s heart stops. It involves discussing care expectations with the patient and family, so a consensus can be reached on treating issues aggressively or palliatively and allow physicians the leeway to avoid unwanted and potentially expensive procedures.
Polypharmacy – defined as regular use of at least five medications – was also noted as an area of concern for practices with patients in long-term care. Only ISNPs and Medicare Advantage plans are responsible for pharmacy costs, but providers on other models are responsible for adverse drug events and outcomes from poor medication management. Studies have shown as the number of medications increases, the risk of an adverse drug event skyrockets – from 13% with two medications, to 58% with five medications, to 80% when seven or more medications are involved..
Tom encouraged PAC physician practices to get involved with the Drive to Deprescribe initiative launched by AMDA in 2021 and consider how they can ease the burden of medication management, as well as prevent the pain and cost of dealing with adverse drug events.
Tom’s presentation offers much more details and insights on how PAC physician practices can approach choosing the right value-based care model. You can listen to the entire recording here.
Learn more about how Netsmart can help your post-acute physician practice transition from fee-for-service to value-based care.
About the Author
Beth Reece, Vice President and General Manager, GEHRIMED
As VP and General Manager, Beth oversees GEHRIMED's day-to-day operations, comprised of products devoted to supporting post-acute and long-term care practies. She proudly serves the PALTC market and ensures our products meet the industry's ever-growing and changing needs. Before GEHRIMED became part of the Netsmart family, she was Chief Financial Officer.






.png)
.png)
